diabetic retinopathy
What is diabetic retinopathy?
Diabetic retinopathy is a complication of diabetes mellitus and is one of the main causes of blindness in young and middle-aged adults today.
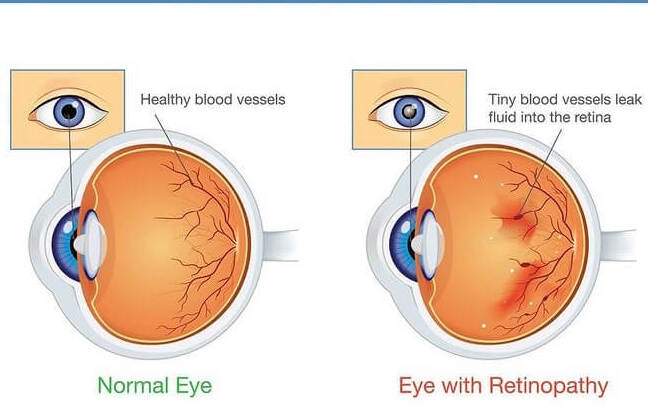
It occurs when diabetes damages the tiny blood vessels inside the retina, the light-sensitive tissue at the back of the eye. A healthy retina is necessary for good vision. Diabetic retinopathy often has no early warning signs. But over time, it can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
What are the types of diabetic retinopathy?
Diabetes affects the peripheral and central retina in different ways. The peripheral retina can be affected by non-proliferative and proliferative diabetic retinopathy. Non-proliferative diabetic retinopathy, also known as background diabetic retinopathy, is the early stage of diabetic retinopathy and occurs when the small retinal blood vessels become affected and start to leak and bleed. At this stage, vision is usually not affected. Proliferative diabetic retinopathy is associated with a high risk of permanent loss of vision. There is growth of abnormal new blood vessels in the retina. These abnormal new vessels can rupture causing significant bleeding that will lead to loss of vision. Progressively, the scar tissues that form can cause retinal detachment. The abnormal blood vessels can grow on the iris and block the outflow of fluid from the eye. Neovascular glaucoma can ensue with a risk of optic nerve damage and blindness.
Who is at risk of developing diabetic retinopathy?
All diabetics are at risk of developing diabetic retinopathy. This is especially so if the diabetes is long-standing. After 20 years, most diabetics will develop this complication of some degree. Those who have poorly controlled diabetes are at higher risk of developing diabetic retinopathy earlier and at more severe stages. People with diabetes should get a comprehensive dilated eye examination or screening at least once a year. If you have diabetic retinopathy, your ophthalmologist can recommend treatment to help prevent its progression.
What are the symptoms of diabetic retinopathy?
Diabetic retinopathy in the early stages has no warning signs and sight may not be affected until the condition is severe. As the disease progresses, symptoms may include the loss of central vision when reading or driving, loss of the ability to see colour, and mild blurring vision. Small spots or floaters may also indicate blood vessel leaks and may clear up in days, weeks, or even months. In the most severe form, with proliferative diabetic retinopathy, there may be sudden severe vision loss from vitreous bleeding or tractional retinal detachment. Because the disease is initially asymptomatic, and can be treated in the earlier stages, it is important to have an eye examination each year, and immediately if you experience any of these symptoms. Late diagnosis and treatment can result in irreversible vision loss.
Can diabetic retinopathy cause vision loss?
Yes. Blood vessels damaged from diabetic retinopathy can cause vision loss. Fragile, abnormal blood vessels can develop and leak blood into the centre of the eye, blurring vision. Diabetic retinopathy can also cause macular oedema. The macula is the central part of the retina that allows for fine details to be seen in the centre of vision. When fluid from blood vessels leaks into the macula, it can swell and result in blurred vision.
Can diabetic retinopathy be prevented?
You cannot completely prevent diabetic retinopathy, however, vision loss can be prevented if it is detected early. You can help protect your sight by having your eyes checked at least once a year by an ophthalmologist or by a retina specialist/surgeon with specialised diabetic retinal photography. You can also help slow down the development of diabetic retinopathy by keeping your blood glucose in check. The HbA1c is a measure of blood sugar level over a three-month period and it should ideally be less than 7 per cent. Other medical conditions such as high blood pressure, high cholesterol and heart disease should be treated and kept under control. Smoking should be stopped and you should exercise regularly. This will reduce your risk of developing diabetic retinopathy.
Is treatment necessary?
If you have macular oedema or severe non-proliferative diabetic retinopathy or proliferative diabetic retinopathy, treatment is necessary. The aim of treatment is to prevent further damage to the retina and further vision loss.
How is diabetic retinopathy treated?
In most cases, laser surgery can prevent significant vision loss associated with diabetic retinopathy. A procedure called laser photocoagulation can be performed to seal or destroy growing or leaking blood vessels in the retina.
• Panretinal photocoagulation (PRP)
This is used to treat the peripheral retina to prevent or stop the growth of the abnormal new blood vessels.
• Focal laser
This is used to treat the macular oedema to reduce the swelling.
In general, each eye requires two to three sessions for a PRP to be completed. You will be expected to go for regular treatments over a period of six to twelve months before diabetic retinopathy is controlled adequately.
In patients with loss of central vision due to diabetic macular oedema, INTRAVITREAL INJECTION of medication into the centre of the eye can reduce the macular swelling and improve vision. Medications which are injected into the eye for diabetic macular oedema include AntiVascular Endothelial Growth Factor (VEGF) drugs such as Avastin, Razumab, and Eylea, as well as steroids. Often, multiple injections at intervals of one month or longer are required to achieve resolution of the swelling. Repeated injections at longer intervals may also be required to maintain the visual improvement. In some people with diabetic retinopathy, the abnormal blood vessels in the retina may also result in massive bleeding into the center of the eye (vitreous humor), causing sudden severe loss of vision. A surgical procedure called a VITRECTOMY can be used to remove the blood that has leaked into this part of the eye.
